Liver Cirrhosis: Incidence, Symptoms, and Treatment
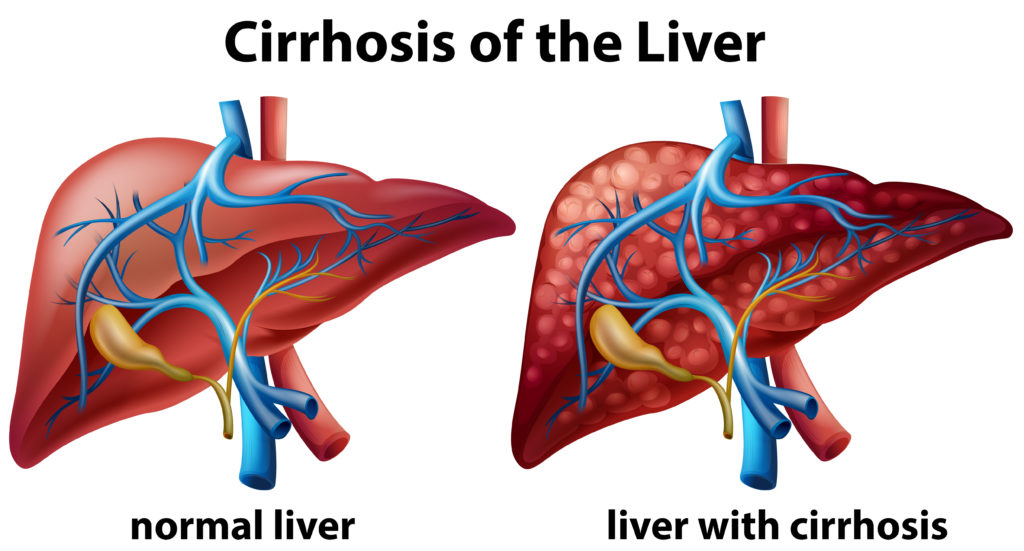
Liver cirrhosis is a late-stage liver disease characterized by scarring (fibrosis) of liver tissue, which disrupts the liver’s ability to function properly. The damage to the liver is progressive and often irreversible, leading to a significant decrease in its ability to process nutrients, hormones, drugs, and toxins, as well as produce proteins and other substances necessary for health. Cirrhosis is the result of long-term, continuous damage to the liver and may be due to many different causes, including chronic alcohol abuse, chronic viral hepatitis (hepatitis B and C), and fatty liver disease associated with obesity and diabetes.
Causes
Common causes of liver cirrhosis include:
- Chronic Alcohol Abuse: A leading cause of cirrhosis. The risk increases with the amount and duration of alcohol consumption.
- Chronic Viral Hepatitis: Particularly hepatitis B and C, which can lead to liver inflammation and, subsequently, cirrhosis.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Associated with obesity, type 2 diabetes, and metabolic syndrome.
- Autoimmune Hepatitis: Where the immune system attacks liver cells, causing inflammation and scarring.
- Other Causes: Can include genetic diseases such as hemochromatosis (iron buildup in the body) and Wilson’s disease (copper accumulation in the liver), bile duct disorders, and certain medications.
Symptoms
In its early stages, cirrhosis often has no symptoms. As the disease progresses, symptoms may include:
- Fatigue and weakness
- Loss of appetite, weight loss
- Nausea, vomiting
- Abdominal pain and bloating (due to fluid accumulation)
- Jaundice (yellowing of the skin and eyes)
- Itching
- Swelling in the legs and ankles (edema)
- Easy bruising and bleeding
- Spider-like blood vessels on the skin
Complications
Cirrhosis can lead to several serious complications, including:
- Portal hypertension: Increased blood pressure in the portal vein, leading to varices (swollen blood vessels) that can bleed.
- Ascites: Accumulation of fluid in the abdomen.
- Hepatic encephalopathy: Impaired brain function due to the liver’s inability to remove toxins from the blood.
- Liver cancer: People with cirrhosis have an increased risk of developing liver cancer.
Diagnosis
Diagnosing cirrhosis involves a combination of medical history, physical examination, blood tests, imaging studies (such as ultrasound, CT scans, or MRI), and sometimes a liver biopsy to assess the extent of liver scarring.
Treatment
There is no cure for cirrhosis, but treatment can help manage symptoms and slow progression. Strategies include:
- Treating the underlying cause: Such as abstaining from alcohol, managing chronic viral hepatitis with antiviral medications, or controlling diabetes.
- Preventing complications: Monitoring and treating complications like portal hypertension, variceal bleeding, ascites, and hepatic encephalopathy.
- Lifestyle changes: Including a healthy diet, avoiding alcohol, and managing weight.
- Liver transplant: In advanced cases, a liver transplant may be considered when the liver function significantly deteriorates.
Prevention
Preventing liver cirrhosis largely involves minimizing risk factors:
- Avoid excessive alcohol consumption.
- Get vaccinated against hepatitis B and practice safe behaviors to reduce the risk of hepatitis C.
- Maintain a healthy weight and manage conditions like diabetes and high cholesterol.
- Avoid exposure to toxins and use medications responsibly.
Early detection and management of liver diseases can help prevent cirrhosis. If you have risk factors for liver disease, regular check-ups and liver health monitoring are crucial.
Why Choose London Private Ultrasound?
At London Private Ultrasound, we prioritize your health and comfort. Our team of experienced radiologists and healthcare professionals are dedicated to providing the highest quality of care. Here’s why you should choose us:
- Expert Radiologists: Our team consists of highly trained and experienced radiologists who are experts in ultrasound diagnostics.
- State-of-the-Art Technology: We use the latest ultrasound machines to ensure the highest level of accuracy in our scans.
- Patient-Centered Care: We focus on creating a comfortable and stress-free environment for our patients.
- Timely Results: We understand the importance of quick diagnosis and provide fast and reliable results.
- Convenient Location: Located in the heart of London, our clinic is easily accessible.
Book Your Ultrasound Scan Today
At London Private Ultrasound, we are committed to providing high-quality diagnostic services with a patient-centered approach. Our expert radiologists and cutting-edge technology ensure that you receive the best possible care.
Don’t wait to get the answers you need. Book your abdomen or pelvic ultrasound scan today by contacting us at:
Address: 27 Welbeck Street, London, W1G 8EN
Tel: 020 7101 3377
You can also schedule an appointment online through our website. Experience the convenience, comfort, and expertise at London Private Ultrasound.
We look forward to assisting you with your healthcare needs and ensuring you receive the best possible diagnostic care.
ExcellentBased on 540 reviews Trustindex verifies that the original source of the review is Google.
Trustindex verifies that the original source of the review is Google. Jackie Supernova2024-07-16excellent service. easy to book and adjust dates if required. The staff are friendly. The clinician was attentive and informative and did a thorough investigation. Highly recommend if you need fast reliable diagnostic results.Trustindex verifies that the original source of the review is Google.
Jackie Supernova2024-07-16excellent service. easy to book and adjust dates if required. The staff are friendly. The clinician was attentive and informative and did a thorough investigation. Highly recommend if you need fast reliable diagnostic results.Trustindex verifies that the original source of the review is Google. Mostafa Hawwash2024-07-16Quick and fast and reliable. Thank youTrustindex verifies that the original source of the review is Google.
Mostafa Hawwash2024-07-16Quick and fast and reliable. Thank youTrustindex verifies that the original source of the review is Google. Aisha Fontaine2024-07-16Reza Farahmandfar, was very professional, my appointment was on time. He explained every step of the way. Definitely will book with him again.Trustindex verifies that the original source of the review is Google.
Aisha Fontaine2024-07-16Reza Farahmandfar, was very professional, my appointment was on time. He explained every step of the way. Definitely will book with him again.Trustindex verifies that the original source of the review is Google. Sammy Andrews2024-07-15Brilliant clinic. I've visited a few the last few years for various issues and London Private Ultrasound was prompt, clean, professional and reassuring. If I need anything else I will definitely go back.Trustindex verifies that the original source of the review is Google.
Sammy Andrews2024-07-15Brilliant clinic. I've visited a few the last few years for various issues and London Private Ultrasound was prompt, clean, professional and reassuring. If I need anything else I will definitely go back.Trustindex verifies that the original source of the review is Google. Matt Mawson2024-07-14Friendly, reassuring, calm manner with a easy to understand explanation of the details. Highly recommended.Trustindex verifies that the original source of the review is Google.
Matt Mawson2024-07-14Friendly, reassuring, calm manner with a easy to understand explanation of the details. Highly recommended.Trustindex verifies that the original source of the review is Google. uday singh2024-07-10I was there for my lower limb ultrasound but the quality of explanation by the doctor was so comprehensive that I decided to get a full body scan. Greatly impressed with the attention and attitude of everyone there. If anyone requires an ultrasound, in my view this is the place.Trustindex verifies that the original source of the review is Google.
uday singh2024-07-10I was there for my lower limb ultrasound but the quality of explanation by the doctor was so comprehensive that I decided to get a full body scan. Greatly impressed with the attention and attitude of everyone there. If anyone requires an ultrasound, in my view this is the place.Trustindex verifies that the original source of the review is Google. Aisha Smith2024-07-09Great experience, got an appointment within an hour. Sonographer was lovely and really reassuring and was useful to be able to see the images on the large screen while lying down.Trustindex verifies that the original source of the review is Google.
Aisha Smith2024-07-09Great experience, got an appointment within an hour. Sonographer was lovely and really reassuring and was useful to be able to see the images on the large screen while lying down.Trustindex verifies that the original source of the review is Google. Joana Macedo2024-07-08Same day scan. Very knowledgeable clinician. Thanks
Joana Macedo2024-07-08Same day scan. Very knowledgeable clinician. Thanks
London Private Ultrasound Clinic
At London Private Ultrasound all our services, our specialists and us using the latest Ultrasound technology is designed to deliver the greatest possible experience for all our patients and visitors.
We are conveniently located in Welbeck Street, a stone’s throw from the famous Harley Street and our clinic is a place where you will be welcomed by our friendly staff and feel comfortable in our safe, clean, and reassuring environment.
Address: 27 Welbeck Street, London, W1G 8EN
Tel: 020 7101 3377


